Coding Workforce Shortages & Solutions: Comprehensive Analysis
The coding workforce crisis is no longer a future concern. Hospitals, physician groups, and billing companies are already losing revenue every month because key coding seats stay vacant, productivity drops, and senior coders burn out. At the same time, payers are tightening rules, ICD-11 accuracy expectations are rising, and every missed code creates measurable leakage across the entire revenue cycle.
This guide maps where shortages are worst, how they hit reimbursement, and which specific solutions actually move the needle, drawing from AMBCI insights on coding errors, revenue leakage, and future-proof roles.
1. Understanding The Scale Of Coding Workforce Shortages In 2025
Coding shortages are not just “open positions.” They show up as delayed claim submission, incomplete documentation, denied high-complexity encounters, and high reliance on expensive contract coders. When unfilled roles intersect with complex reimbursement rules, hospitals see a double hit: lower top-line revenue and higher administrative cost. AMBCI’s work on hospital reimbursement by specialty shows that specialties with intense coding complexity feel the pain first.
Workforce gaps are most visible in roles linked to denial prevention, risk adjustment, and emerging virtual care. Organizations that monitor coding accuracy impact on revenue often discover that their “staff shortage” is actually a mix of unfilled roles, under-skilled coders, and weak use of automation. Without a clear map of required roles, it is impossible to align hiring with the revenue cycle KPIs that leadership cares about.
Before we talk solutions, you need a precise picture of which roles matter, what they own, and how success will be measured. The following AMBCI-style map does exactly that and connects directly to topics like denials management best practices and financial audit readiness.
| Role (Hire Title) | Core Mandate / Primary KPI | Ideal Background / Training Focus |
|---|---|---|
| CDI–Coding Quality Analyst | Close documentation gaps; improve E/M accuracy; reduce CO-50 denials. | Strong CDI plus deep knowledge of ICD-11 guidelines and [ICD-11 coding rules] alignment. |
| Denials Analytics Lead | Cut avoidable coding denials by 25–35%; maintain payer-specific playbooks. | Excel / BI skills, familiarity with [denials management best practices] data sets. |
| Risk Adjustment Coder (HCC) | Raise RAF with fully supported HCC capture; zero unsupported diagnoses. | Advanced chronic condition coding and [ICD-11 guideline](https://ambci.org/medical-billing-and-coding-certification-blog/guide-to-icd-11-official-coding-guidelines-explained) mastery. |
| Telehealth Coding SME | Correct POS and modifier use; no POS denials on virtual care. | Telehealth policy knowledge and [medical claims terminology](https://ambci.org/medical-billing-and-coding-certification-blog/medical-claims-submission-complete-terminology-guide). |
| Outpatient Surgery Coding Lead | Accurate APC assignment; maintain OR case turnaround within two days. | CPT surgery expertise plus [specialty specific terms](https://ambci.org/medical-billing-and-coding-certification-blog/chiropractic-coding-amp-billing-terms-comprehensive-guide). |
| Inpatient Coding Auditor | Audit high-value DRGs; protect against take-backs and audit findings. | DRG grouping, [financial audit readiness](https://ambci.org/medical-billing-and-coding-certification-blog/guide-to-financial-audits-in-medical-billing). |
| ProFee Coding Specialist | Optimize professional fees; reduce under-coding in evaluation services. | Strong E/M, multi-specialty exposure, familiarity with [reimbursement models](https://ambci.org/medical-billing-and-coding-certification-blog/predicting-changes-in-healthcare-reimbursement-models-by-2027). |
| Revenue Integrity Analyst | Identify missing charges and bundling errors; protect high-margin services. | Charge description master skills plus [revenue leakage](https://ambci.org/medical-billing-and-coding-certification-blog/revenue-leakage-in-medical-billing-original-industry-data-amp-insights) analysis. |
| Charge Capture Specialist | Ensure every billable service reaches the claim; monitor late charges. | Workflow mapping with [RCM efficiency](https://ambci.org/medical-billing-and-coding-certification-blog/revenue-cycle-management-efficiency-original-metrics-amp-benchmarks-report) benchmarks. |
| Coding Education Specialist | Reduce repeat coder errors by 40%; run targeted micro-trainings. | Teaching skills plus reference to [medical billing dictionary](https://ambci.org/medical-billing-and-coding-certification-blog/medical-billing-dictionary-common-terms-amp-definitions) and [compliance dictionary](https://ambci.org/medical-billing-and-coding-certification-blog/medical-coding-compliance-dictionary-essential-terms). |
| Coding Operations Manager | Hit daily productivity and quality SLAs across all specialties. | People leadership, dashboard use, and [salary benchmarks](https://ambci.org/medical-billing-and-coding-certification-blog/2025-medical-coding-salary-guide-state-by-state-breakdown) awareness. |
| RCM Data Analyst (Coding Focus) | Turn coding KPIs into dashboards; flag patterns that hurt reimbursement. | SQL or BI tools with grounding in [RCM metrics](https://ambci.org/medical-billing-and-coding-certification-blog/revenue-cycle-management-efficiency-original-metrics-amp-benchmarks-report). |
| Automation Workflow Specialist | Deploy coding assist tools without increasing compliance risk. | Knowledge of [future innovations in billing software](https://ambci.org/medical-billing-and-coding-certification-blog/future-innovations-in-medical-billing-software-amp-financial-management). |
| Coding Quality & Compliance Officer | Keep audit findings below threshold; maintain policy traceability. | Regulatory mindset plus [compliance terminology](https://ambci.org/medical-billing-and-coding-certification-blog/medical-coding-compliance-dictionary-essential-terms). |
| Provider Education Liaison | Coach physicians on documentation that supports accurate coding. | Communication skills and [coding educator roadmap](https://ambci.org/medical-billing-and-coding-certification-blog/career-roadmap-how-to-become-a-medical-coding-educator). |
| DME Coding Specialist | Accurate DME modifiers and medical necessity support. | Deep knowledge of [DME coding rules](https://ambci.org/medical-billing-and-coding-certification-blog/guide-to-durable-medical-equipment-dme-coding). |
| Chiropractic Coding SME | Correct use of chiropractic codes; prevent medical necessity denials. | Experience with [chiropractic coding guidance](https://ambci.org/medical-billing-and-coding-certification-blog/chiropractic-coding-amp-billing-terms-comprehensive-guide). |
| Coding Denials Navigator | Own end-to-end appeal strategy for coding denials. | Knowledge of [denials playbooks](https://ambci.org/medical-billing-and-coding-certification-blog/coding-denials-management-comprehensive-analysis-amp-best-practices) and payer policies. |
| Pre-Bill Audit Specialist | Catch high-risk errors before claims go out. | Checklist design using [common error lists](https://ambci.org/medical-billing-and-coding-certification-blog/top-10-most-common-medical-coding-errors-and-how-to-avoid-them). |
| Remote Coding Team Lead | Coordinate distributed coders, ensure consistent quality and security. | Remote leadership skills with insight from [LinkedIn leader Q&A](https://ambci.org/medical-billing-and-coding-certification-blog/linkedin-qampa-how-healthcare-leaders-are-navigating-the-2025-billing-landscape). |
| Multi-Specialty Coding Generalist | Cover gaps across multiple outpatient clinics. | Broad training path aligned with [step-by-step career guides](https://ambci.org/medical-billing-and-coding-certification-blog/step-by-step-guide-starting-a-career-in-medical-billing-and-coding). |
| Specialty Coding Expert (Oncology/Cardiology) | Protect high-value specialty revenue and reduce niche denials. | Advanced disease coding plus [ICD-11 nuance](https://ambci.org/medical-billing-and-coding-certification-blog/impact-of-accurate-icd-11-coding-on-reimbursement-rates-2025-study). |
| Payment Integrity Analyst (Coding) | Identify payer underpayments tied to coding disputes. | Contract reading skills with [reimbursement trend](https://ambci.org/medical-billing-and-coding-certification-blog/predicting-changes-in-healthcare-reimbursement-models-by-2027) awareness. |
| Coding Workforce Planner | Forecast future coding FTE needs and skills mix. | Uses [emerging job role insights](https://ambci.org/medical-billing-and-coding-certification-blog/top-emerging-job-roles-for-certified-medical-coders-2025-insights) and salary data. |
| Clinical Coding Trainer & Mentor | Convert new graduates into productive coders within 6 months. | Grounded in [educator AMAs](https://ambci.org/medical-billing-and-coding-certification-blog/medical-billing-amp-coding-educators-ama-how-to-pass-your-certification-exams) and continuing education best practices. |
2. 2025 Emerging Coding Roles And KPIs Hiring Managers Care About
Once you see the roles in one view, patterns appear. Shortages are most severe in positions that sit at the intersection of coding, analytics, and payer strategy. Many leaders still hire only “general coders” even though their biggest revenue risk sits in HCC capture, denials analytics, and pre-bill audit. AMBCI’s articles on revenue leakage and RCM benchmarks make clear that these specialists pay for themselves quickly.
High demand roles usually map to a few KPI families: denial rate, days in accounts receivable, case mix index stability, RAF lift, audit outcomes, and coder productivity per FTE. When you write job descriptions that tie directly to these KPIs, you attract more serious candidates, especially those already tracking their impact as described in AMBCI’s career roadmap for CPCs and CBCS salary guides. Organizations that still post generic “medical coder” roles will lose the talent war to employers who speak the language of measurable impact.
3. Root Causes Behind The Coding Workforce Gap
There is no single driver behind the shortage. The first is a simple pipeline issue. Many potential coders still do not understand that entry paths exist, even though AMBCI’s step-by-step career guide and dictionary resources show that people without clinical backgrounds can enter successfully. Employers expect “two to three years of experience” for roles that could be trained in twelve months with structured mentoring.
The second driver is a skills mismatch. Coding complexity has increased with ICD-11 implementation, new bundled payment models, and specialty-specific rules. Yet many coders receive only broad introductory training. They struggle when confronted with advanced risk adjustment, DME rules, or chiropractic documentation, topics explored in AMBCI’s DME and chiropractic coding guides.
Third, burnout is chronic. Coders sit between providers who want speed and payers who demand perfect compliance. When organizations treat coding as pure “production work,” ignore continuing education, and block flexible remote options, their most experienced people leave for competitors or independent contracting. The pipeline then loses mentors who would have trained the next generation.
Quick Poll: What’s your biggest blocker to solving your coding workforce shortage?
4. Operational Solutions To Stabilize Coding Capacity
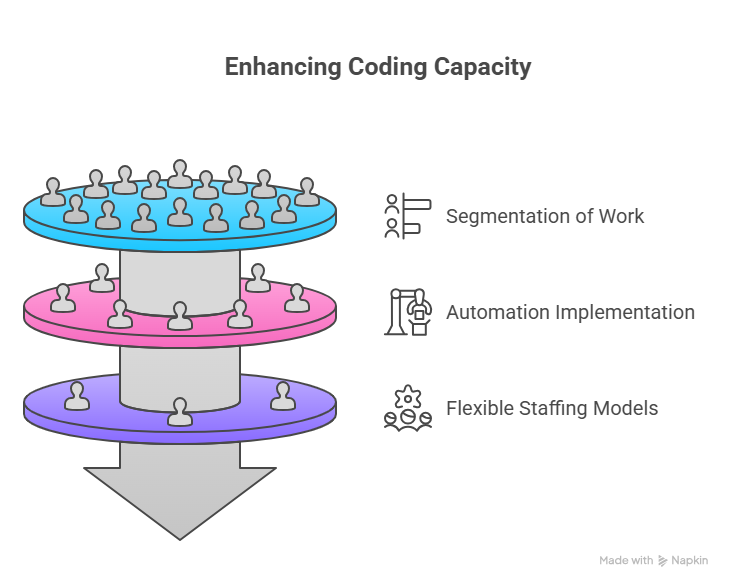
Shortage problems improve only when they are tied to operational levers. The first lever is segmentation of work. Instead of asking every coder to handle every task, break the flow into standardized lanes: high-complexity audit, routine outpatient, denials appeals, pre-bill review, and specialty coding. This mirrors the role structure in the earlier table and aligns neatly with AMBCI’s material on denials management, claims submission terminology, and revenue cycle metrics.
The second lever is intentional use of automation. Tools that suggest codes or flag incomplete documentation can raise throughput, but they must be deployed with clear guardrails that follow coding compliance dictionaries and financial audit guidance. Automation should remove repetitive clicks, not replace coder judgment. When coders see tools as support rather than threat, retention improves.
A third lever is flexible staffing models. Build hybrid teams that mix full-time in-house coders with vetted remote specialists and outsourced partners for peak periods. The best organizations track talent availability the way they track payer contracts, using insights from leader Q&A discussions and Reddit AMA summaries. This approach turns staffing from a reactive scramble into a planned capacity strategy tied to seasonal volumes and service line growth.
5. Building Long Term Talent Pipelines With Education And Career Pathways
Solving shortages in a durable way requires more than filling current vacancies. You need a pipeline that begins with entry-level talent and extends through senior specialist and leadership roles. AMBCI’s career roadmap for CPCs and CBCS salary guide illustrate how clear pathways motivate coders to stay long enough to recoup training investment.
Start by partnering with education providers that align with AMBCI’s exam prep strategies and continuing education frameworks. Offer structured progression: trainee coder, associate coder, senior coder, specialist, team lead, and educator. Each step should carry distinct responsibilities, pay bands informed by the state-by-state salary data, and access to focused upskilling in areas such as risk adjustment, DME, or telehealth.
You can also make your organization attractive by signaling future-ready work. Highlight opportunities to work with innovative billing software, automation, and analytics. Coders who read AMBCI’s insights on jobs thriving with automation want employers that will not leave them behind as technology advances. When your recruitment messaging reflects these pathways, you tap into a broader pool of ambitious candidates who view coding as a long term profession instead of a short stop.
Finally, close the loop by nurturing internal educators. Support experienced coders who want to follow the medical coding educator roadmap or participate in AMBCI’s educator AMAs. When training is delivered by respected peers who understand your environment, new hires ramp faster and your workforce becomes self-sustaining.
6. FAQs: Coding Workforce Shortages And Practical Solutions
-
Unfilled or under-skilled coding roles delay charge capture, push claims submission into later billing cycles, and increase avoidable denials. Studies like AMBCI’s work on coding accuracy and hospital revenue show that even small declines in quality produce significant drops in reimbursement for complex service lines. When denials rise, staff spend more time on appeals rather than clean claim generation, which further strains capacity. Over time, the organization absorbs higher write-offs, increased audit risk, and lower margins across specialties as highlighted in specialty reimbursement analyses.
-
Begin with a focused set of indicators: clean claim rate, denial rate for coding-related reasons, coder productivity by encounter type, audit accuracy, and backlog days for charts awaiting coding. AMBCI’s revenue cycle metrics report provides useful benchmark ranges. Track these by specialty and payer so you can see where shortages hurt most. Add talent-specific metrics such as vacancy duration, turnover rate for coders, time to full productivity for new hires, and training hours completed. When these indicators move together, you can tell whether investments in training, automation, or outsourcing are actually stabilizing capacity.
-
Smaller organizations win by designing roles that offer autonomy, flexibility, and focused growth rather than simply higher pay. For example, you can build remote or hybrid arrangements, predictable schedules, and exposure to interesting multi-specialty cases informed by AMBCI’s salary benchmark data. Offer paid time for continuing education and support for certification prep that uses exam strategy guides. Emphasize a collaborative culture where coders partner closely with providers and RCM leaders, which many professionals value more than incremental salary increments at large systems.
-
Create a structured, layered training program that leverages curated content rather than ad-hoc shadowing. Begin with foundational terminology through AMBCI’s billing and compliance dictionaries, followed by service-line-specific modules using resources on ICD-11 guidelines, DME, or chiropractic coding. Assign practice cases with automated feedback before exposing trainees to live claims. Senior coders then spend focused time on targeted reviews, not basic terminology or simple errors, which preserves their energy and accelerates the overall learning curve.
-
Treat automation as a “second set of eyes,” not a replacement for coders. Start with tools that flag missing documentation, inconsistent modifiers, or incomplete problem lists. Use AMBCI’s insights on future billing innovations and reimbursement model shifts to design guardrails that maintain compliance. Involve coders in tool selection and workflow design, and provide transparent quality dashboards. When coders see that automation removes tedious tasks, supports accurate coding, and respects official ICD-11 rules, they are far more likely to embrace it, which improves both morale and audit readiness.
-
Clear career paths are one of the strongest retention levers. When coders understand how to move from entry-level roles into specialist, lead, or educator positions, they are more willing to stay through the steep early learning period. AMBCI’s CPC roadmap, automation-ready job insights, and educator career guides give concrete templates. By investing in internal educators who use resources like AMBCI’s educator AMA, you create continuous learning inside your own walls. That reduces dependence on external hiring and turns your organization into a magnet for ambitious coders who want long term growth.
-
Monitor three signals: payer policy changes, regulatory updates, and technology adoption curves. AMBCI’s forward-looking content on reimbursement model predictions, software innovation, and emerging coder job roles is designed to help leaders see these shifts early. Build workforce plans that assume ongoing complexity growth: more hierarchical codes, new quality programs, and continued automation pressure. When you align training, hiring, and technology around these signals, you protect your organization from surprise shocks and convert future change into competitive advantage.