Value-Based Care Coding Terms Explained
Value-Based Care (VBC) isn’t a “future trend.” It’s the system quietly deciding which organizations get bonuses, which get penalties, and which get forced into thinner margins year after year. In VBC, coding is no longer just about getting a claim paid—it’s about proving patient complexity, validating outcomes, and protecting reimbursement across an entire performance year. If your documentation is weak, your risk capture erodes. If your coding doesn’t align with measures, your quality score drops. This guide explains VBC coding terms in plain language—so you can stop guessing and start coding like revenue depends on it.
1) Value-Based Care Coding: What Changes and Why It’s Hard
In fee-for-service billing, your world is “one claim, one payment.” In value-based care, your world becomes “one patient, one year, one scorecard.” That shift breaks a lot of teams because they keep working like the old system—reacting to denials, chasing missing info late, and treating diagnosis capture as optional instead of strategic.
Here’s what VBC changes for coders and billers:
Coding becomes longitudinal. A diagnosis that matters in January still matters in November. If it disappears from documentation, risk models can drop it. That’s why teams that don’t understand documentation standards get crushed by audits and recapture requirements. Tight alignment with clinical documentation improvement (CDI) terminology and clinical documentation integrity concepts stops risk leakage.
Payment becomes model-based, not visit-based. A claim can pay perfectly, yet you still lose revenue because your patient risk score is understated. That’s the invisible loss most billing teams never catch until leadership asks why bonuses didn’t show up. If your analytics aren’t connected to revenue cycle efficiency benchmarks, you won’t even see the erosion.
Quality reporting becomes a coding problem. Measures fail when services were done but not coded/linked correctly—especially when diagnosis-to-procedure logic isn’t clean. Teams fighting “mysterious gaps” usually have basic workflow holes in medical claims submission terminology and messy reporting pipelines tied to electronic claims processing terms.
Audit risk becomes constant. Value-based contracts attract audits because risk scores and quality metrics affect payer spend. If your organization can’t produce defensible support, you’ll see clawbacks and compliance exposure. Get serious about compliance audit trends and what enforcement looks like in billing compliance violations and penalties.
The hard truth: VBC punishes teams who treat coding like data entry. You’re doing financial reporting with clinical evidence. And if you don’t treat it that way, someone else (payer, auditor, employer coalition) will do it for you—with your revenue.
| Term | Clear Definition | Coding / Billing Impact |
|---|---|---|
| Value-Based Care (VBC) | Payment tied to outcomes, quality, and efficiency | Coding affects scores and long-term reimbursement |
| Quality Measure | A tracked metric (screenings, control rates, follow-ups) | Wrong linkage causes measure failure despite care delivered |
| Risk Adjustment | Payment changes based on patient complexity | Under-documentation quietly lowers reimbursement |
| HCC | Hierarchical Condition Category grouping of diagnoses | Controls which chronic conditions increase risk score |
| RAF Score | Risk Adjustment Factor derived from coded conditions | Lower RAF = lower benchmark payments |
| Performance Year | Measurement period used to score quality/risk | Late coding fixes may not count after close |
| Attribution | Assignment of a patient to a provider/group | Defines who is “responsible” for gaps and cost |
| Care Gap | Missing recommended service or follow-up | Gap closure depends on correct coding + documentation |
| MEAT | Monitor/Evaluate/Assess/Treat support for diagnoses | Weak MEAT triggers audit removals and clawbacks |
| Suspected Condition | Potential diagnosis not clinically confirmed | Risk coding requires defensible evidence—avoid speculation |
| Problem List Integrity | Accuracy of chronic conditions carried in the EHR | Dirty lists cause under/over-coding and audit risk |
| ICD-10/ICD-11 Specificity | Granularity required to represent complexity correctly | Non-specific coding lowers risk capture and measure accuracy |
| Z Codes (SDOH) | Social determinants of health coding | Supports population health and care management programs |
| Numerator | Count of patients meeting a measure requirement | Coding drives whether patient “counts” as compliant |
| Denominator | Total eligible patients for the measure | Wrong exclusions inflate failure rates |
| Exclusion | Valid reason a patient should not be counted | Requires documentation + correct coding to apply |
| Benchmark | Target cost/quality threshold used for scoring | Risk + quality accuracy influences benchmark comparison |
| Shared Savings | Bonus when costs are below benchmark with quality met | Poor coding can erase bonus eligibility |
| Downside Risk | Penalty exposure when costs exceed benchmark | Bad risk capture makes performance look worse than reality |
| Registry Reporting | Submitting measure data to a registry/QCDR | Coding errors break reporting and score submission |
| Risk Recapture | Re-documenting chronic conditions annually | Missing recapture causes RAF decline year over year |
| Chart Review | Retrospective review to validate conditions/measures | Finds missed HCCs and measure leakage |
| Prospective Review | Pre-visit identification of gaps and suspect conditions | Improves capture without post-visit scrambling |
| Coding Leakage | Care performed but not counted due to coding/reporting miss | Causes score failure with no “denial” signal |
| Audit Trail | Record of edits, submissions, and documentation history | Protects against disputes and supports defense |
| ERA/EOB Reconciliation | Matching payer adjudication to internal posting | Prevents false balances and bad A/R decisions |
| A/R Aging (VBC Impact) | How long balances remain unpaid | Delayed corrections reduce measure windows and cash flow |
| Compliance Exposure | Risk of penalties from inaccurate billing/documentation | Higher in VBC due to risk score sensitivity |
2) Risk Adjustment, HCCs, and RAF: The Terms That Control Your Money
If you only learn one VBC concept deeply, make it risk adjustment. It’s where organizations lose the most money quietly because the claim still pays and nobody screams. But the benchmark drops, the RAF declines, and leadership wonders why “we’re working harder for less.”
Risk Adjustment means payers adjust expected cost and payment based on how complex your patients are. Complexity is proven through accurate diagnosis capture, defensible documentation, and correct code selection—supported by CDI logic from CDI terms and documentation frameworks like clinical documentation integrity terms.
HCC (Hierarchical Condition Category)
An HCC is a payer model grouping that converts diagnoses into risk categories. Not every diagnosis creates risk uplift. HCC models prioritize high-cost, chronic, and complicated conditions. That’s why vague coding kills you—you lose the “weight” that matches patient reality.
RAF (Risk Adjustment Factor)
RAF is the numeric score representing expected patient cost. Higher RAF generally means higher expected spend, which means higher payment benchmarks—when properly supported. It’s why MEAT-level support matters and why weak documentation turns into audit vulnerability.
The annual recapture trap
Most risk models require annual capture. If the condition isn’t documented and coded again within the performance year, it can drop off. That’s not “unfair.” That’s how the rules work. If your workflow doesn’t build in structured capture, your RAF erodes every year and you lose money even with the same patients.
Coders should treat this like a scheduled operational system, not random chart clean-up. Build risk capture processes the same way you build denial workflows using coding audit trails and quality controls from coding QA.
Why teams fail here
Provider documentation lacks specificity
Conditions are listed but not supported
Chronic conditions aren’t reassessed
Problem lists are copy/pasted without clinical support
Coders avoid queries due to time pressure
Those issues show up later as findings in compliance audits, financial hits in revenue cycle efficiency reporting, and increased error visibility through industry coding error rate analysis.
3) Quality Measures, Measure Leakage, and Coding Alignment
Quality measures are where “we did the work” still becomes “we scored as if we didn’t.” That’s measure leakage. It destroys incentives, harms network performance, and makes organizations look clinically sloppy when the real issue is documentation and coding alignment.
Numerator, denominator, exclusions — why these terms matter
Denominator: everyone eligible for the measure
Numerator: who successfully completed it
Exclusion: valid reason to remove from scoring
Coders impact all three. A wrong exclusion means a patient stays in the denominator and drags your score down. A missing code means the numerator never gets credit.
Measure alignment also depends on clean claim flow fundamentals: submission accuracy, reporting readiness, and reconciliation discipline using medical claims submission terms and adjudication understanding through the EOB guide.
Common measure leakage patterns
Preventive service performed but not linked to the right diagnosis
Screening documented in a note but not captured in the billing data
Follow-up happens but gets coded under generic visit logic
Chronic disease control documented but missing supporting evidence
Telehealth services coded inconsistently, disrupting reporting pipelines
If your team already struggles with fast-changing reimbursement realities, pair your VBC training with the reality checks inside telemedicine reimbursement trends and the compliance implications of HIPAA changes.
The “looks fine” trap
VBC performance can look fine day-to-day because claims still pay. The damage shows up at the end of the year when incentives are calculated. That’s why VBC coding requires proactive review systems and operational monitoring built on RCM efficiency benchmarks and A/R truth from A/R terminology.
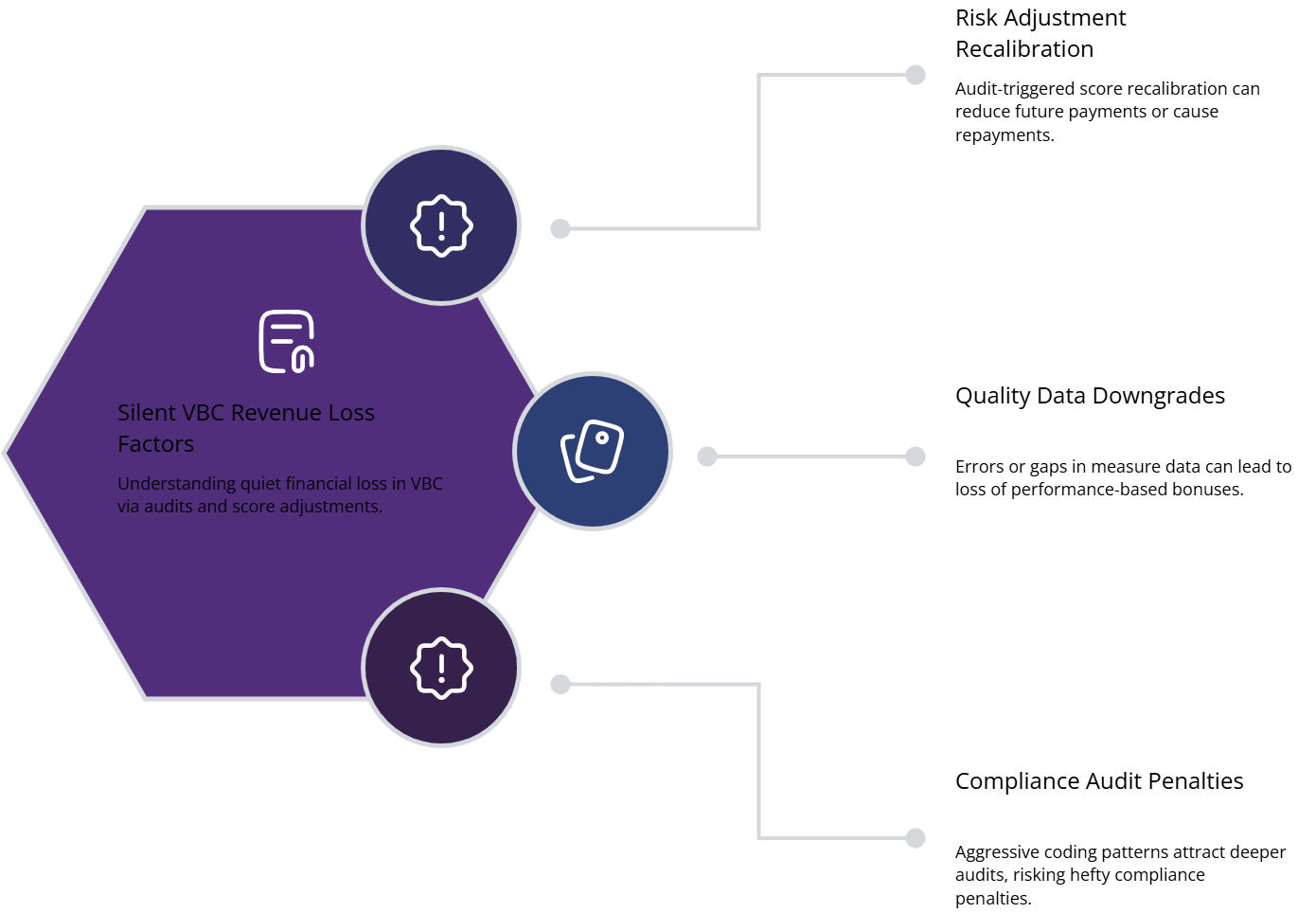
4) VBC Denials You Don’t See: Audits, Clawbacks, and Silent Revenue Loss
Traditional denials are loud. They show up as unpaid claims. VBC losses are quiet. You get paid—then later lose money through score recalculation, audit findings, and benchmark adjustments.
The three “silent denial” buckets
1) Risk score clawbacks
If an auditor determines conditions were not supported, they can remove diagnoses and recalculate risk. That triggers repayment or future payment reduction. This is why documentation discipline must be treated like compliance, with awareness shaped by audit trails and signals from audit trend reporting.
2) Quality score downgrades
If measure data is missing, miscoded, or misreported, you fail performance. Bonuses shrink or disappear. This is common when teams don’t interpret payer feedback correctly using EOB logic and don’t manage operational truth inside A/R reporting.
3) Compliance penalties and contract pressure
VBC attracts compliance focus because organizations can profit by overstating complexity. If a payer sees patterns that look aggressive, you’ll face deeper audits. That risk is explained clearly in compliance violations and penalties and reinforced by regulatory impact reporting.
The real pain point most teams ignore
The cost of VBC errors isn’t only money. It’s operational chaos:
Rework cycles
Provider friction
Patient confusion
Delayed outreach
Broken reporting
That chaos shows up in productivity strain, which connects to coding productivity benchmarks and workforce realities like coding workforce shortage analysis.
5) The Practical VBC Coding Playbook: How to Build a System That Scores
Value-based coding success is not “hire one expert.” That creates a single point of failure. You need a repeatable system that turns risk capture and measure alignment into a workflow.
Step 1: Build a VBC-ready documentation engine
Train providers and CDI teams to document conditions with specificity and support. Use consistent language through CDI terms and reinforce integrity through documentation integrity terms.
Step 2: Run prospective “gap + suspect” prep before visits
Pre-visit prep prevents post-visit begging. Identify:
suspect HCCs needing confirmation
care gaps needing closure
missing labs/screenings
outdated problem list items
This is where coding becomes strategy, not cleanup.
Step 3: Do quarterly risk recapture reviews
Don’t wait for December. Your year-end rush creates errors and audit exposure. Quarterly review protects RAF stability and reduces denial noise later.
Step 4: Treat measure leakage like denial management
If care happened but didn’t count, that’s functionally a denial of credit. Create a leakage queue the same way you’d create a denial workqueue. Tie it to operational truth using RCM efficiency metrics and reconcile impacts through A/R terms.
Step 5: Standardize tech + terminology
If your team doesn’t speak the same language, reports become meaningless. Use a shared reference like coding software terminology and ensure data capture aligns to claims pipelines in electronic claims processing terms.
Step 6: Monitor your “VBC health dashboard”
Track:
RAF trend by provider
HCC capture rate
gap closure velocity
measure leakage volume
audit findings frequency
Then connect these to staffing and training insights from workforce demographics reporting and remote workforce trends.
6) FAQs: Value-Based Care Coding Terms and Real-World Fixes
-
Value-based care pays providers based on outcomes and quality, not just services. For coders, that means your work affects risk scores, quality measures, incentives, and penalties—not only claim payment. A diagnosis that is documented poorly can reduce RAF and lower future benchmarks even if the visit paid normally.
-
Standard diagnosis coding supports medical necessity and claim accuracy. HCC coding supports risk adjustment and payment modeling. HCCs require stronger documentation support because they impact future reimbursement and are frequently audited. That’s why teams must align to CDI standards and maintain defensible workflows through audit trail practices.
-
Measure leakage is when care happens but your reporting doesn’t get credit—because coding, linkage, or documentation is missing. The patient stays in the denominator but never hits the numerator, so performance drops. Leakage is one of the most common reasons teams miss incentives even when clinicians are doing the right care.
-
Because claims still pay. The real consequences show up at reconciliation time: bonus reductions, benchmark adjustments, and audit findings. That’s why you must track VBC performance continuously using RCM benchmark thinking and reconcile impacts through A/R controls.
-
Improve documentation quality and specificity, not aggression. Focus on conditions that are clearly present, clinically addressed, and MEAT-supported. Use structured CDI queries when needed and standardize documentation expectations using documentation integrity terminology.
-
Common issues include: unsupported chronic conditions copied forward, vague diagnosis descriptions, missing assessment/treatment evidence, and absence of medical decision-making support for the condition coded. Audit pressure and repayment exposure are strongly linked to patterns described in compliance audit trends and consequences outlined in compliance penalties reporting.